🌱Regulation as the Root: Building Bridges Between OT & ABA
An Interview with an Occupational Therapist on Interdisciplinary Care
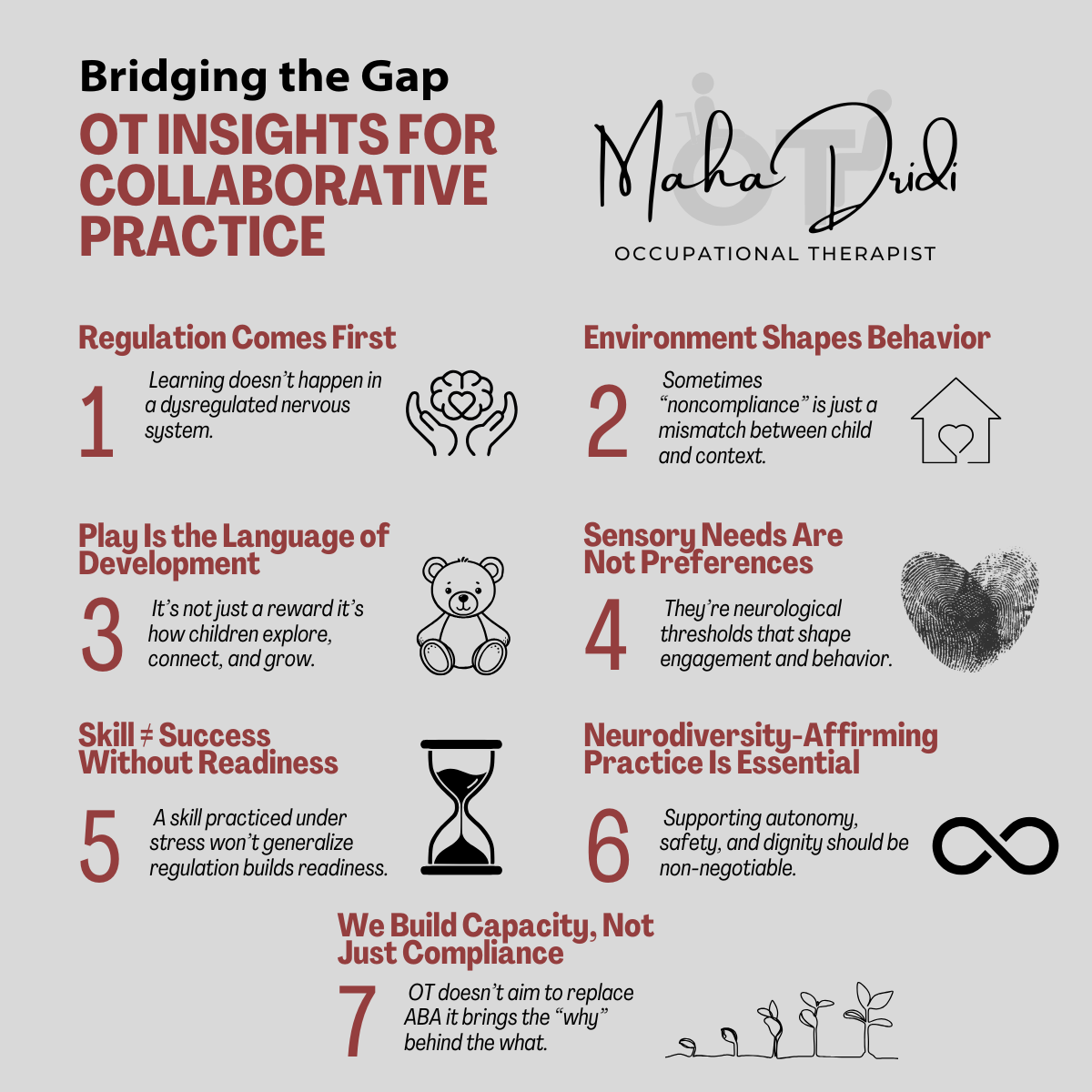
When it comes to supporting children with complex needs, no single discipline holds all the answers. That’s why meaningful collaboration between occupational therapists (OTs) and behavior analysts (BCBAs) is not just beneficial—it’s essential.
In this interview, I had the opportunity to speak with an experienced pediatric OT who brings a sensory-informed, strengths-based lens to her work. Together, we explored how OT and ABA can move beyond parallel practice and into true partnership—rooted in regulation, shared curiosity, and respect for each child’s individual needs.
Whether you're a BCBA looking to deepen interdisciplinary collaboration or simply curious about how OT complements behavior analytic care, this conversation offers insight, practical examples, and a powerful reminder: regulation is the root of meaningful growth.
Professional Bio
Maha Dridi is a licensed Occupational Therapist (BSc OT, OTR/L), Applied Behavior Analysis Technician (ABAT), and Certified Cognitive Remediation Therapy(CRT) with over 10 years of experience working across the lifespan from early childhood to adulthood. She is a Senior OT Consultant, Neuro & Pediatric Rehabilitation Specialist, and founder of a therapy clinic focused on inclusive, evidence-based care. Maha brings extensive international experience, having worked across a variety of healthcare, educational, and community settings in both local and global contexts. Her approach blends neurodevelopmental and cognitive rehabilitation frameworks with a strengths-based, person-centered philosophy. She is also a published therapy content creator whose educational guides and visuals are used and shared by professionals and families worldwide.
1. How would you describe occupational therapy (OT) to someone who isn’t familiar with it?
Occupational therapy helps people engage meaningfully in the daily activities or “occupations” that matter most to them. For children, those include play, self-care, learning, emotional regulation, and social participation. We use activity-based, holistic strategies to help children build the physical, sensory, and emotional capacities needed to thrive.
💡Insight: OT meets kids where they are developmentally, not just where a program says they “should” be.
3. How do you typically assess a child’s needs, and how does that differ from or complement a behavior analytic approach?
OT assessments look at how a child functions in meaningful, real-life contexts. I assess sensory processing, motor skills, visual perception, attention, regulation, and task performance through standardized tools, clinical observation, and caregiver input. While ABA assessments often focus on observable behaviors and environmental contingencies, OT explores the underlying developmental and neurophysiological foundations.
💡Insight: OT assessments are designed not only to see what a child does but to understand why it’s hard, and how to make it easier.
2. What are some common misconceptions you encounter about OT, especially from those in other helping professions like ABA?
OT is often misunderstood as simply “the handwriting therapy” or “the sensory play service.” In reality, we address everything from executive function to feeding, emotional regulation to body awareness. Another common misconception is that OT is passive or less evidence-based. On the contrary, our work is guided by neuroscience, standardized assessments, and clinical reasoning grounded in both research and function.
💡Insight: Just because an OT session looks like play doesn’t mean it’s not targeted, intentional, and evidence-informed.
4. What are your main goals when working with children, and how do those align or differ from the goals BCBAs often have?
My goals focus on independence and participation. Can the child engage in meaningful routines like dressing, toileting, playing with peers, and participating in the classroom? BCBAs often work toward skill acquisition and behavior reduction, and while those goals may overlap, OT adds the lens of regulation, sensory readiness, and developmental appropriateness.
💡Insight: A skill practiced under stress may not generalize. OT builds readiness, so the skill can actually stick.
6. What areas of development do you address that you feel are sometimes overlooked in behavior analytic programming?
OT often addresses body awareness, co-regulation, interception, reflex integration, and postural stability areas that are foundational to participation but not always represented in behavior plans. We also deeply value play not just as reinforcement, but as a developmental necessity and therapeutic modality.
💡Insight: A child’s “readiness” to comply or engage isn’t just a behavioral state; it’s often a sensory and nervous system state.
5. Can you share an example of how OT and ABA can work hand-in-hand to support a client?
I worked with a child struggling with transitions and dressing. The ABA team used visual schedules and reinforcement systems, while I focused on sensory tolerance, motor sequencing, and environmental modifications. When we aligned our strategies using sensory prep before transitions and simplifying dressing tasks, the child’s meltdowns decreased, and independence improved.
💡Insight: When we view the same challenge through different lenses, we often find better solutions together.
7. What can BCBAs do to improve collaboration and communication with OTs on shared cases?
“Collaboration allows us to see the whole child—not just through one lens, but through many that sharpen our understanding.”
Engage early, observe each other’s sessions, and be open to blending approaches. Using shared, child-centered language goes a long way, for example, saying “What helps this child feel safe and successful?” rather than “What motivates them?” also opens up more inclusive conversation.
💡Insight: Collaboration starts with mutual respect, but it thrives with shared curiosity.
9. What’s one thing you wish every BCBA knew about OT?
That OT isn’t just an add-on; it’s often a missing piece. We don’t just address behavior; we support the why behind it. We don’t just build skills; we build the capacity to use them in real life. OT values function, regulation, and joy equally, and we want to be active collaborators, not competing voices.
💡Insight: OT isn’t the “alternative.” It’s part of a complete support system for kids with complex needs.
8. How does your training in sensory processing influence your work with clients, and what do you wish more BCBAs understood about sensory needs?
Sensory processing influences how a child interprets and interacts with their world, how they sit, eat, move, and focus. My training helps me recognize when behaviors stem from overstimulation, under-responsiveness, or sensory avoidance. I wish more BCBAs viewed sensory needs not as preferences but as neurological thresholds that impact behavior, attention, and regulation.
💡Insight: You can’t reinforce your way out of a sensory meltdown. You have to support the nervous system.
10. If a BCBA wanted to learn more about OT, where would you recommend they start (books, courses, podcasts, etc.)?
The Out-of-Sync Child by Carol Stock Kranowitz
Sensational Kids by Lucy Jane Miller
Two Sides of the Spectrum podcast (by OT Meg Proctor)
The STAR Institute (for sensory processing research & training)
My website: https://mahedridi.com: I share free guides, practical OT strategies, and real-world examples of interdisciplinary care
💡Insight: Learning from OTs starts with listening to our lived clinical experiences, then building together.
A heartfelt thank-you to Maha Dridi, OTR/L, for sharing her time, insight, and compassion in this conversation. Her ability to bridge clinical knowledge with child-centered care is a powerful reminder of what’s possible when professionals work together with respect and shared purpose.
To explore more of Maha’s work—including free guides, practical OT strategies, and real-world examples of interdisciplinary care—visit her website at https://mahedridi.com/
A Note to Readers:
Want to share your perspective? I’d love to feature guest posts - whether you’re a practitioner, parent, educator, or someone with lived experience. Use the contact form below to connect!
*Disclaimer: The views expressed in this blog are my own (Functionally Speaking ABA) and do not reflect the views of UNMC